Pain is defined as any unpleasant sensation experienced by an individual. Hyperglycemia or high sugar levels are the main cause for chronic pain in diabetic individuals. Hyperglycemia causes
Polyol pathway hyperactivity
Decreased insulin secretion or insulin resistance, is responsible for the enhanced of the polyol pathway activity.
Oxidative and nitrosative stress
Initiated by autoxidation of glucose and their metabolites, increased intracellular formation of AGEs, increased expression of the receptor for AGEs and its activating ligands, altered mitochondrial function, activation of PKC isoforms and overactivity of the hexosamine pathway
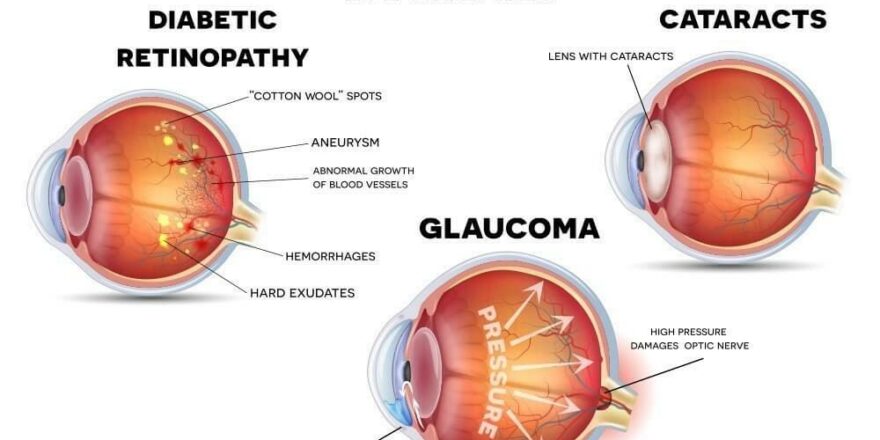
Microvascular changes
Peripheral perfusion is reduced, not only in the nervous tissue, but also in the skin, being an important physiological evidence of microvasculature alteration. As a result, nerve ischemia occurs, caused by raise in wall thickness and hyalinization of the basal lamina of vessels that nurse peripheral nerves, together with luminal reduction
Channels sprouting
Disturbed action potentials are produced by damaged nerve endings, being interpreted by the central nervous system (CNS) as pain or dysesthesias. Changes in ion channel expression in peripheral fibers are direct consequences of nerve injury, leading to hyperexcitability, that is far linked with neuropathic pain
Microglial activation
Diabetes is associated with a reduction in glial fibrillary acidic protein (i.e., glial fibrillary acidic protein) immunoreactive astrocytes in the spinal cord, which may affect the functional support and role of astrocytic cells in the nervous tissue, such as the clearance of neurotransmitters within the synaptic cleft
Central sensitization
Primary afferents are sensitized, inducing dorsal horn hyperactivity and neuroplastic changes in central sensory neurons. Allodynia commonly occurs in diabetic patients.
Brain plasticity
Functional changes in pain processing areas of the CNS, besides the spinal cord, have been ultimately linked, in a tight relation to increased peripheral input. Among these areas, marked changes in the thalamus, cortex and rostroventromedial medulla (RVM) have been reported in many diabetic patients.
The ventral posterolateral nucleus (VPL) of the thalamus is the main receiving area of nociceptive stimuli that is processed in the spinal cord. Projection neurons reach the thalamus trough the spinothalamic tract (STT), which represents a major ascending nociceptive pathway. The hyperexcitability of STT neurons probably accounts to hypersensitivity to external stimuli and spontaneous pain, increased in primary afferents activity and to plastic changes in spinal neurons.
Thus, pain and diabetes are very closely linked. A diabetic rehabilitation program focuses both on managing the pain with the help of manual therapy, advanced electrotherapy and pain management therapies along with a program to help normalize the blood glucose levels. Thus, one must consult a Diabetic Rehabilitation Specialist to help manage the pain and normalize blood sugar levels.